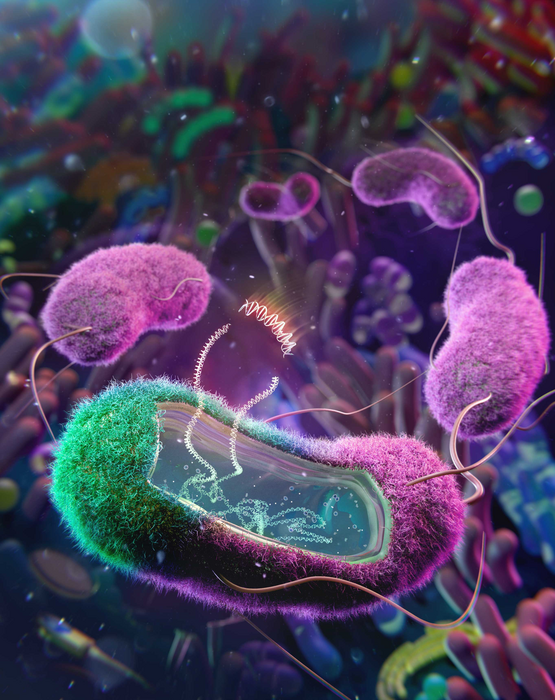
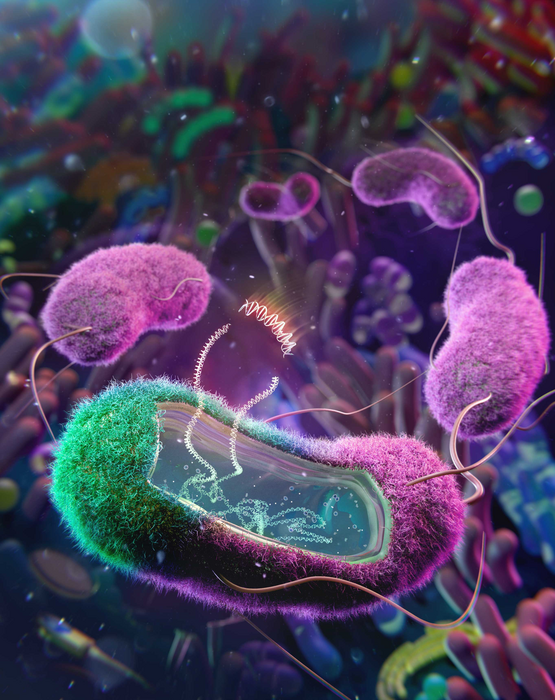
Scientists have long tried to introduce genetically engineered bacteria into the gut to treat diseases. In the past, these attempts have focused on engineering common lab strains of E. coli, which cannot compete with the native gut bacteria that are well adapted to their host. Now, a group of researchers from the University of California, San Diego, successfully engineered E. coli collected from both human and mice gut microbiomes and showed that they have the potential to treat diseases such as diabetes. Their finds are publishing in the journal Cell.
“All I can say to the non-native bacteria is good luck. The gut microbiome is very dynamic and is constantly changing, making things even harder for the non-native bacteria,” says Amir Zarrinpar (@Zarrinparlab), a gastroenterologist at UC San Diego Health and the senior researcher of the paper. “It is challenging for bacteria that have never lived inside of a mammal before to now go into the gut microbiome jungle with all of these hostile conditions that are geared towards preventing bacterial invaders from taking hold.”
The group devised a solution to this problem by directly engineering E. coli collected from the hosts. “Bacteria in our body are adapted to each one of us specifically: the kind of foods we eat, the common stresses our body experiences or induces, and our genetic background,” says Zarrinpar. “This constantly fluctuating environment is their normal.” This is a big advantage for native bacteria and makes them ideal candidates for engineering.
“We have engineered these bacteria to become factories that can live in our microbiome and potentially produce medicines,” says Zarrinpar. “We know that E. coli can pick up pathogenic genes and cause disease, and now we’re just realizing that if we put a beneficial gene in, it can help us to treat chronic diseases, maybe even cure some of them.”
The team first collected stool samples from the host and extracted E. coli for further modifications. “We say to the bacteria: Hey, we will give you a new superpower, which you may not even benefit from, but we will put you right back into the environment that you thrive in,” says Zarrinpar.
The superpower that the team gave to these specific bacteria is a protein called bile salt hydrolase (BSH). After a single treatment in mice, E. coli with BSH were found throughout the entire gut of the mice and they retained their BSH activity for the entire lifetime of the host. The group also show that the BSH activity was able to positively influence diabetes progression in mice.
This is a significant improvement over similar treatments with non-native laboratory strains of engineered bacteria, where more than one treatment is often required. And these engineered bacteria do not stay in the host’s gut for nearly as long as, or as consistently as, the native E. coli method identified by Professor Zarrinpar’s team.
In addition to successfully influencing diabetes in mice, the group was also able to make a similar modification to E. coli extracted from human gut.
While they have demonstrated substantial results, engineering native bacteria comes with another set of challenges. “Native bacteria are very resistant to modifications; it is part of their innate defense mechanism,” says Zarrinpar. Their data suggest that inserting a gene into a native bacterium has about 100-fold lower success rate than doing so with lab strain bacteria, but Zarrinpar and his team are optimizing this process. “There are many new genetic engineering tools available now that will allow us to engineer these bacteria more effectively,” says Zarrinpar.
The group is planning on using this technology to find ways to treat more diseases. “We are dreaming big,” says Zarrinpar. “This technology is something that can potentially open up the application of the microbiome therapy to influence so many different chronic and genetic diseases.”