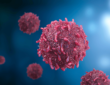
Sickle cell disease (SCD) is a genetic blood disorder characterized by misshapen red blood cells, leading to various complications such as pain episodes, organ damage, and reduced life expectancy. Over the years, significant strides have been in SCD treatment, ranging from traditional therapies to cutting-edge gene editing techniques. In this article, we will explore the latest advancements in SCD treatment options, including oral medications, gene therapies, and potential future innovations.
Advancements in Oral Medications:
Recent developments in oral medications have offered new hope for SCD patients. Pfizer’s GBT021601, acquired through Global Blood Therapeutics, is one such promising drug. By preventing the sickling of red blood cells, GBT021601 aims to alleviate symptoms and improve patients’ quality of life. Its accessibility and ease of administration make it a potential game-changer in SCD treatment, offering a more convenient alternative to traditional therapies.
Furthermore, the success of GBT021601 underscores the importance of ongoing research and development in the field of small molecule drugs. Companies like Fulcrum Therapeutics are exploring novel approaches to induce fetal hemoglobin expression, a strategy with the potential to revolutionize SCD treatment. Despite challenges in development, such as regulatory hurdles and safety concerns, these advancements represent significant progress towards addressing the unmet needs of SCD patients.
Gene Therapies:
In addition to oral medications, gene therapies have emerged as a promising avenue for treating SCD. Casgevy and Lyfgenia are two groundbreaking therapies that have gained regulatory approval in recent years. Developed through collaboration between leading biotech companies, these therapies aim to correct the underlying genetic mutation responsible for SCD.
Casgevy, a CRISPR-based gene editing therapy, has demonstrated remarkable efficacy in clinical trials, offering hope for patients with severe forms of the disease. Similarly, Lyfgenia, an ex vivo-engineered cell therapy, has shown promising results in improving patients’ outcomes. While therapies hold immense potential, their limited scalability and high cost pose challenges in ensuring widespread access for all SCD patients.
Future Innovations:
Looking ahead, researchers are exploring innovative approaches to further enhance SCD treatment outcomes. In vivo gene editing therapy, a long-term ambition of many in the field, holds promise for offering a one-time, curative treatment for SCD. Partnerships between academic institutions and philanthropic organizations, such as the Innovative Genomics Institute and Pioneer Science, are paving the way for the development of next-generation therapies.
Moreover, advancements in delivery technologies, such as CRISPR-based editing systems, are opening new possibilities for in vivo gene therapy. These innovations have the potential to transform the landscape of SCD treatment, offering hope for a future where effective therapies are accessible to all patients, regardless of their geographical location or socioeconomic status.
Conclusion:
In conclusion, advancements in SCD treatment have brought renewed optimism for patients and clinicians alike. From oral medications to cutting-edge gene therapies, researchers are continuously pushing the boundaries of what is possible in treating this complex genetic disorder. While challenges remain, such as ensuring equitable access to innovative therapies and addressing safety concerns, the progress made thus far underscores the importance of ongoing investment and collaboration in the field of hematology. With continued research and development, we can strive towards a future where SCD is no longer a life-threatening condition, but a manageable disease with effective treatment options for all patients.